Understanding Inflammatory Bowel Disease
What Is Inflammatory Bowel Disease?
Inflammatory Bowel Disease (IBD) is the term for several chronic disorders that can cause inflammation in the gastrointestinal tract. The two main types of IBD are Crohn’s disease and ulcerative colitis, both of which involve problems with the immune system.
IBD can affect people of all ages, but is most often diagnosed in teens and young adults. It can present in varying degrees of severity and is a lifelong condition, but can be managed and may even go into remission for long periods.
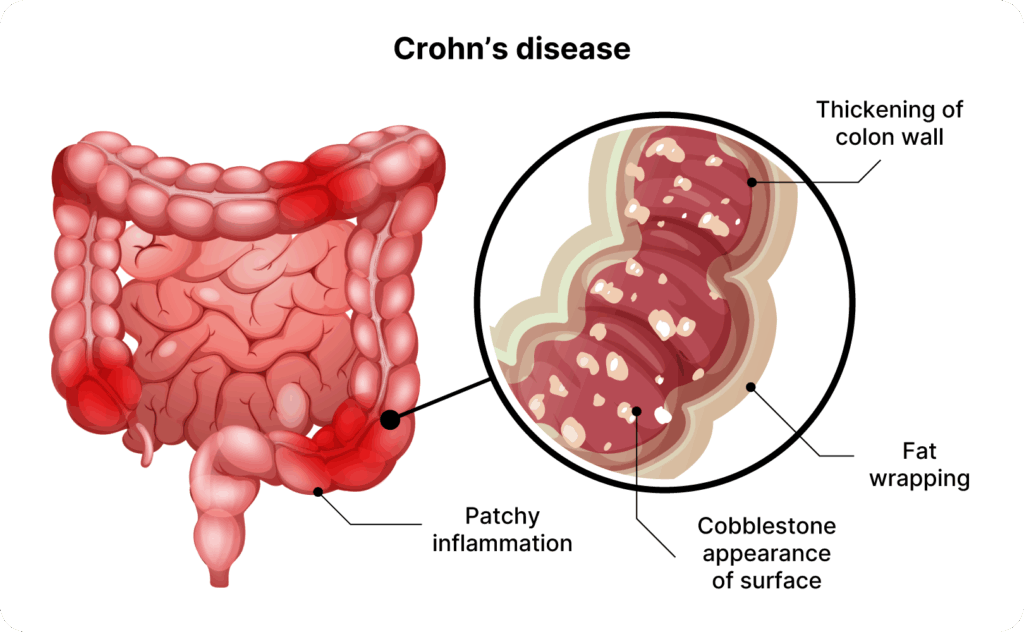
Crohn’s Disease
This disorder often affects the small intestine and colon, but can affect any part of the digestive tract. In some cases, the inflammation it causes can extend through the entirety of the bowel wall.
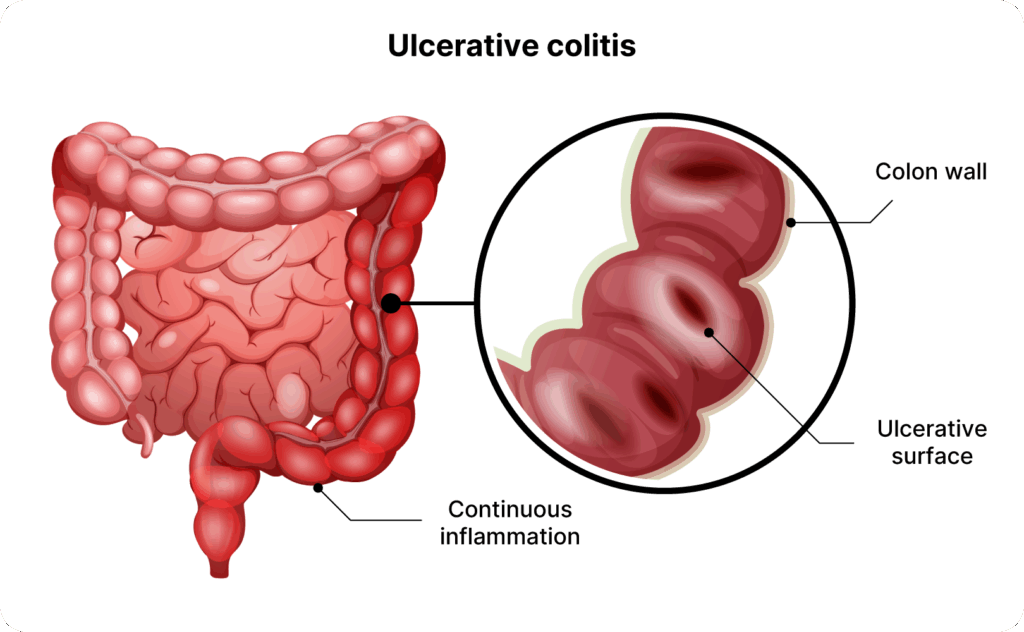
Ulcerative Colitis
Ulcerative colitis causes inflammation that is limited to the colon (large intestine) and rectum. It affects only the innermost lining of the bowel and can cause ulcers in these areas.
Causes and Risk Factors of Inflammatory Bowel Disease
The exact causes of IBD are not fully understood, but current research suggests the disease develops from a combination of factors. These appear to prompt the immune system into attacking the intestinal lining, leading to chronic inflammation:
- Immune system triggers like a virus, bacteria, or a change in the gut microbiome
- Environmental factors like growing up in sterile environments with limited germ exposure, certain early-life infections, or frequent antibiotic use in infancy
- Genetic predisposition such as having certain genetic markers or a family history of IBD
There are also several risk factors that increase the chance of developing IBD:
- Having a family history of IBD
- Smoking, which appears to increase the risk of Crohn’s, but carries a slightly lower risk of ulcerative colitis
- Use of Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) like ibuprofen, naproxen, or diclofenac, which may worsen existing IBD or trigger flares in some patients
Signs and Symptoms of Inflammatory Bowel Disease
IBD can cause a variety of digestive symptoms. Their severity and characteristics can differ from person to person.
Here are the symptoms of inflammatory bowel disease:
- Abdominal pain and cramping
- Anaemia (a low red blood cell count)
- Change in bowel habits
- Chronic diarrhoea (frequent loose or watery bowel movements)
- Constantly feeling fatigue or weakness
- Fever or night sweats
- Growth delays in children or delayed puberty
- Incontinence (inability to control bowel movements)
- Rectal bleeding (blood in your stools or on the toilet tissue)
- Unexplained weight loss and loss of appetite
Get Assessed and Diagnosed for IBD
If you believe you may have IBD or are experiencing the symptoms listed above, let our specialist assess you for early diagnosis and treatment.
How Inflammatory Bowel Disease Is Diagnosed
Your doctor usually will begin your clinical evaluation with a request for your medical history and ask about the symptoms you’re experiencing.
You may also be asked to undergo diagnostic tests like these:
- Blood tests: These look for signs of inflammation like elevated C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR), signs of anaemia or nutrient deficiencies (like low iron or B12), and signs of specific antibodies associated with IBD.
- Stool tests: Stool samples are taken and sent to a lab to check for infection and rule out bacteria or parasites as the cause of symptoms. Faecal calprotectin testing may also be used to distinguish IBD from non-inflammatory conditions like irritable bowel syndrome (IBS).
- Colonoscopy/sigmoidoscopy: A flexible camera is inserted through the anus to examine the colon and rectum. It allows a doctor to see inflammation, ulcers, or bleeding. It also allows the doctor to take tissue samples (biopsies) to confirm IBD.
- Imaging scans: CT and MRI scans may be used to view the small intestine and check for strictures (narrowed segments), fistulas, or abscesses. These are signs of Crohn’s disease.

- Imaging scans: CT and MRI scans may be used to view the small intestine and check for strictures (narrowed segments), fistulas, or abscesses. These are signs of Crohn’s disease.
Potential Complications of Inflammatory Bowel Disease
As inflammatory bowel disease advances, complications can occur. These include:
- Intestinal strictures: Narrowed segments of bowel developed when chronic inflammation causes scar tissue buildup in the intestinal walls. This makes it difficult for food to pass through the intestine. It can even cause a blockage (bowel obstruction), which requires urgent treatment.
- Fistulas: Abnormal tunnels or passageways formed when inflammation penetrates the intestinal wall and connects to another organ or to the skin. Fistulas can lead to leakage of bowel contents into other parts of the body, causing infections.
- Abscesses: Pockets of pus in the abdominal cavity or around the anal area, often as a complication of fistulas or severe inflammation, these can cause severe pain and fever.
- Ulcers and perforation: Long-term inflammation can lead to sores or deep ulcers that penetrate the intestinal wall. In rare cases, severe ulceration can lead to a perforated colon (a hole in the colon wall) that leaks intestinal contents into the abdomen.
- Toxic megacolon: A segment of the colon becomes acutely and severely dilated and inflamed, causing the colon to stop moving gas and faeces. This leads to rapid swelling of the abdomen and systemic toxicity. This is life-threatening and requires emergency treatment.
- Colon cancer: Chronic inflammation increases the long-term risk of developing colorectal cancer.
Treatment of Inflammatory Bowel Disease
Treatment depends on the type of IBD, the areas of the gut involved, and the severity of the disease. Treatment often starts with milder therapies and moves to stronger ones only if needed.
Non-Surgical Management
This is usually the first-line therapy for IBD. Several options are available, including these:
- Anti-inflammatory drugs: Given orally or rectally, these work by locally reducing inflammation in the gut lining. They are most effective in mild to moderate ulcerative colitis and some mild Crohn’s cases if disease is limited to the colon. For moderate to severe flares of IBD, corticosteroids are commonly used to quickly calm a flare by suppressing the immune response.
- Immune system suppressors: These target the underlying immune response causing the inflammation. These drugs don’t provide instant relief but can help prevent the immune attacks on the gut when taken long-term.
- Antibiotics: These are used to manage complications like infections, but are not used as primary long-term treatment for IBD itself.
- Lifestyle and dietary management: Avoiding trigger foods and adjusting fibre intake can help manage the chronic diarrhoea associated with IBD.
Surgical Treatments
Surgery is needed when certain complications arise or the disease does not respond to more conservative medical therapy. The options include these:
- Colectomy: Partial colectomy is the removal of the colon and rectum. After removal of the colon, the surgeon may create an ileal pouch to store waste internally or create a stoma (an opening on the abdomen) for stool to exit into a disposable bag. In some cases, the entire colon is removed (total colectomy), often for those with severe ulcerative colitis.
- Bowel resection: The surgeon removes the diseased segment of intestine and then connects the healthy ends back together in a process called anastomosis.
- Strictureplasty: This procedure widens the narrowed section by surgically opening and reshaping it, all without removing any part of the bowel. This is typically done for patients with multiple strictures or those who have already had large sections of bowel removed. This is because the procedure tries to preserve intestinal length.
- Fistula and abscess surgery: Crohn’s disease near the anus often causes fistulas that tunnel from inside the rectum to the skin around the anus. This surgical procedure is done to drain the abscess of such fistulas and remove the fistula tract, which can prevent further abscess formation.
Your doctor will discuss the expected recovery time after the surgery, which is typically several weeks. You will also learn if you need additional procedures (like the creation of a temporary stoma) or further treatments after surgery.
Recovery and Prognosis for IBD
The recovery varies by type of treatment. Patients who have undergone surgery typically spend about 1-2 weeks in the hospital and several weeks at home regaining strength. If you have a temporary stoma, you will learn stoma care before going home.
Consistency with treatment is key to a good prognosis for IBD. It tends to be a relapsing-remitting illness.
Individuals who adhere to their maintenance medications are much less likely to see relapses. Those who have regular follow-ups or check-ins with their gastroenterologist or colorectal specialist also benefit from improved management.
Periodic blood tests, stool tests, and even scheduled colonoscopies can be useful as well. The last test can help check for early signs of colorectal cancer, which IBD patients are at higher risk for.
For surgical treatment, the prognosis is generally good:
- Ulcerative colitis patients who undergo colectomy are essentially free from colitis flares as the disease no longer affects them without the colon.
- Surgery for Crohn’s disease patients can significantly improve symptoms and resolve complications. However, Crohn’s can recur, so ongoing medication is often recommended to reduce recurrence risk.
Prevention and Management Tips
Early detection and healthy lifestyle habits can lower your risk of inflammatory bowel disease. Below are some tips that may help you manage it.
- Take medications as prescribed: Once you’re in remission, staying on your maintenance medication greatly increases the chances of avoiding a relapse. Skipping doses or stopping treatment without guidance often leads to a flare.
- Watch your diet and hydration: Pay attention to foods that trigger your symptoms. Ensure you drink plenty of fluids to stay hydrated, especially if you have chronic diarrhoea.
- Avoid NSAIDs and be cautious with other meds: Common over-the-counter pain relievers like ibuprofen, naproxen, or aspirin can irritate the gut. Consult your doctor for alternatives.
- Regular follow-up visits: Perform routine check-ins with your gastroenterologist or colorectal specialist, periodic blood tests or stool tests to monitor inflammation, and scheduled colonoscopies to screen for early signs of colon cancer.
- Stay active and manage stress: Exercise regularly and manage stress, as high stress may trigger digestive symptoms via the brain-gut connection.
- Avoid smoking: Avoiding tobacco can improve Crohn’s disease outcomes and lower complication rates.
- Limit alcohol: If consumed, do so in moderation.
- Family history: Tell your doctor if you have close relatives with IBD, as you may need earlier or more frequent screening depending on that.
Schedule an Appointment for IBD Screening
Consult our colorectal specialist for a thorough consultation and diagnosis if you have concerns about IBD. We can provide an early evaluation and propose a tailored treatment plan if needed.
