Piles Surgery
What Is Piles Surgery and Why Is It Needed?
Piles surgery is a procedure used to remove or reduce haemorrhoids, also called piles. These refer to swollen blood vessels in or around the anus that can cause pain, bleeding, itching, or prolapse. These swollen vessels also typically protrude during bowel movements.
Non-surgical treatments for piles include topical medications and rubber band ligation. Piles removal surgery is only offered after the non-surgical options have failed, complications have arisen, or the case is severe. Examples of such cases are ones where the prolapsed internal piles hang out of the anus or external piles have painful blood clots.
The surgery aims to remove or shrink problematic haemorrhoid tissue. The exact approach used will depend on the severity of the patient’s symptoms, location of the haemorrhoids or risk of complications.
Non-Surgical Approaches or Procedures
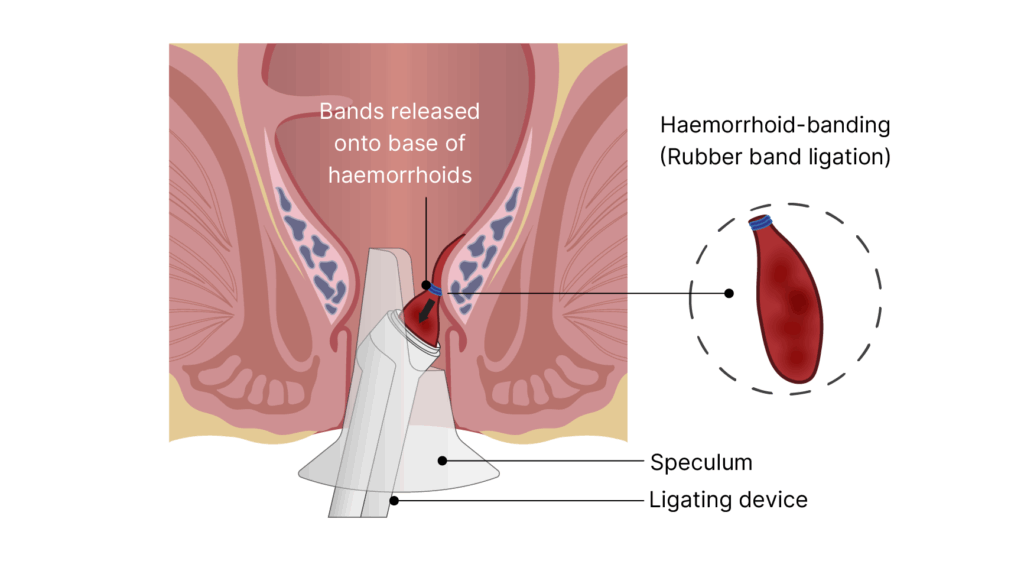
There are two non-surgical procedures that are effective for early-stage or small haemorrhoids: rubber band ligation and sclerotherapy.
Rubber band ligation involves placing a tight rubber band around the base of the haemorrhoid to cut off its blood supply until it withers and falls off. Sclerotherapy involves injecting a chemical solution into the haemorrhoid to make it shrink in several sessions.
Haemorrhoidal Artery Ligation (THD)
This is also known as Transanal Hemorrhoidal Dearterialisation (THD), and is often preferred for Grade II or III haemorrhoids due to its minimally invasive nature. It tackles piles by tying off the arteries feeding the haemorrhoids using sutures. Because it doesn’t involve cutting out tissue, it often leads to a quicker recovery time.
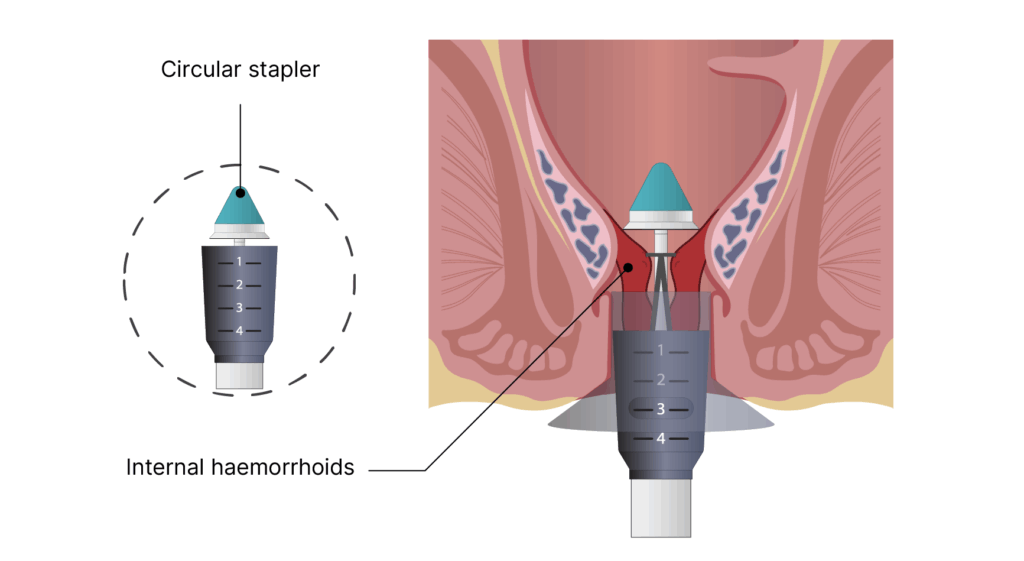
Stapled Haemorrhoidectomy (Stapled Haemorrhoidopexy)
This is a less invasive surgical technique that is typically used for prolapsed internal haemorrhoids but not for external piles. The ring of tissue above the piles is removed and stapled to pull the piles upwards, stopping blood flow. The piles then shrink over time.
Haemorrhoidectomy (Excisional Surgery)
This is the most common option for treating more severe or advanced piles, as it involves excisions or surgical removal of haemorrhoids. The tissue is cut out and the blood vessels supplying it tied off for permanent removal.
Haemorrhoidectomies are typically used for Grade III or Grade IV piles. Larger, more complex cases are more likely to require this approach.
When to Consider Piles Surgery
You may want to consider surgery if your haemorrhoid is interfering with your lifestyle or causing discomfort. Surgery is typically recommended for patients experiencing severe symptoms like bleeding, itching, and prolapse.
A doctor will need to assess if your situation requires surgical intervention already. It is generally advised to consider surgery if more conservative or nonsurgical treatments have already failed. If you are at high risk of developing complications, your doctor may also advise early intervention for better outcomes, especially as haemorrhoids tend to worsen.
Consult a Specialist on Your Treatment Options
Book a consultation with us to get evaluated and learn about your specific treatment options as early as possible.
What to Expect from Piles Surgery
Before the Surgery
During your pre-op consultation, our colorectal specialist will examine you before recommending a treatment plan for your condition. This will include explanations of the procedure, goals, risks, and prep and aftercare instructions, as well as pre-procedure rules you’ll need to follow before the surgery, such as fasting or medication.
At this stage, you can ask questions or raise concerns with us during this consultation, and we will do our best to address each one. Our team will also run through all of the pre-surgery and post-surgery instructions with you.
During the Surgery
Piles surgery can be performed under either local or general anaesthesia, depending on the severity and type of haemorrhoids. Most excisional procedures are done under general anaesthesia. While some complex cases may require a short hospital stay of 1 to 2 days, the majority of patients are discharged on the same day.
The general procedure often takes an hour and is as follows:
- Finding the haemorrhoids
- Excising or cutting out the haemorrhoidal tissue
- Tying off or sealing the blood vessels to the haemorrhoid
- Leaving the surgical site open or suturing it closed
After the Surgery
Piles removal surgery is often an outpatient procedure, but some patients may be asked to stay up to 2 days in the hospital after it. Your doctor will provide aftercare instructions as well as schedule follow-up appointments to keep an eye on your progress.
If you experience any of the following, however, you should contact your doctor immediately.
- Chills
- Difficulty urinating
- Excessive or sustained bleeding through your bandages
- Fever (temperature above 38°C)
- Inability to pass gas/stool
- Persistent nausea/vomiting or dizziness
- Severe abdominal swelling
- Severe pain not controlled by medication
Recovery and Prognosis for Piles Surgery
Since piles surgery is usually done as a day procedure, most patients can go home on the same day. If you were under general anaesthesia for the surgery, you should not drive home after the procedure and ideally have someone accompany you for safety reasons.
Post-procedure care improves outcomes and can shorten recovery timelines, but the usual timeline involves downtime of 1-2 weeks. After that, patients can often return to light activities, but should hold off on strenuous exercise for around 4 weeks. Full recovery is typically achieved in 4-6 weeks.
These are some common aftercare steps you may be advised to follow:
- Keep the area clean and dry, avoid rubbing
- Take warm sitz baths to keep the area clean after a bowel movement.
- Take prebiotics or fibre supplements with ample water to keep your stools soft.
- Avoid prolonged sitting on the toilet or holding in stools
Most patients experience long-term or permanent relief of symptoms. Surgical treatments provide symptom relief, faster recovery and a lowered chance of recurrence as compared to conservative, non-surgical treatment methods.
Risk and Side Effects of Piles Surgery
While piles surgery is a common procedure for haemorrhoid treatment, it has its risks and possible side effects, like all other surgeries:
- Infection after surgery, which can be mitigated with antibiotics
- Short-term post-operative pain, light bleeding, or trouble urinating
- Haemorrhoid recurrence (or growth of new haemorrhoids)
- In rare cases, anal incontinence and anal stenosis
Surgery Fees and Insurance Coverage
For a detailed fee breakdown or to check your eligibility for insurance or Medisave claims, please get in touch with us.
Discuss Your Treatment Options with a Specialist
If you’ve been diagnosed with haemorrhoids or are experiencing ongoing discomfort, speak with our specialist to find out if surgery is right for you.
